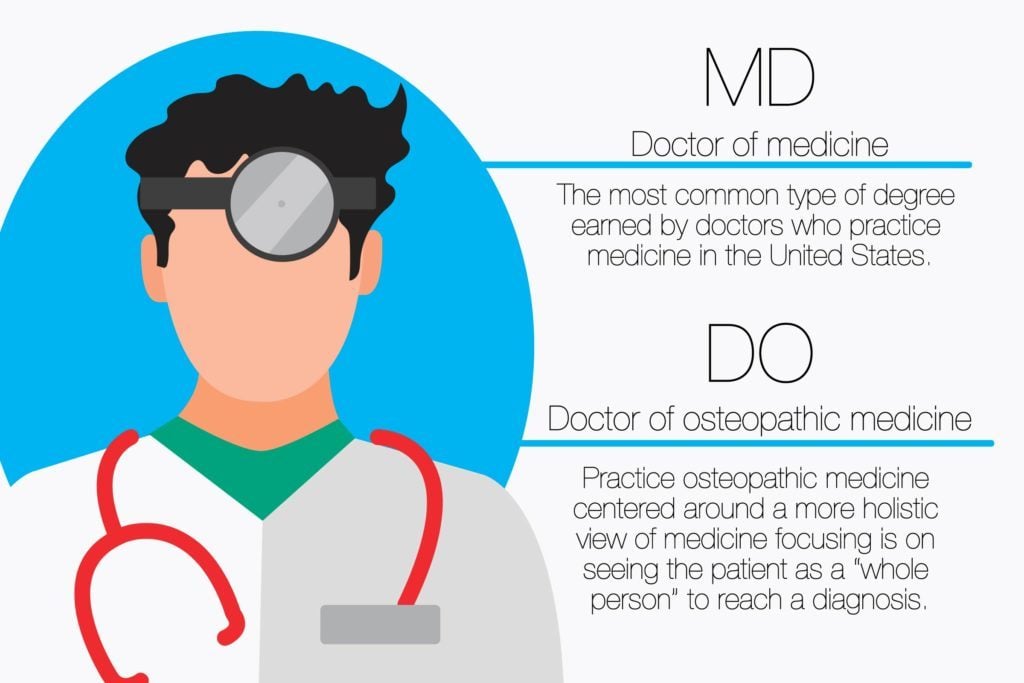
In the realm of healthcare, understanding the difference between an MD and a DO is crucial for informed decision-making. An MD (Medical Doctor) and a DO (Doctor of Osteopathic Medicine) are both licensed physicians who provide medical care, yet they have distinct educational backgrounds and philosophical approaches.
Both MDs and DOs undergo rigorous training, including medical school and residency programs. However, DOs receive additional training in osteopathic manipulative treatment (OMT), a hands-on approach that emphasizes the body's musculoskeletal system and its impact on overall health. This holistic perspective sets DOs apart, allowing them to address the root causes of illness and promote self-healing.
As healthcare continues to evolve, the distinction between MDs and DOs remains relevant. This article delves into the nuances of their education, practice, and the ongoing convergence of medical approaches, providing valuable insights for patients seeking optimal healthcare.
Difference Between MD and DO
The distinction between MDs and DOs encompasses several key aspects that shape their respective approaches to medical care. Understanding these differences is essential for informed decision-making regarding healthcare providers.
- Education: MDs attend allopathic medical schools, while DOs attend osteopathic medical schools.
- Osteopathic Manipulative Treatment (OMT): DOs receive additional training in OMT, a hands-on technique that focuses on the musculoskeletal system.
- Holistic Approach: DOs emphasize a holistic approach to medicine, considering the whole person, not just their symptoms.
- Scope of Practice: Both MDs and DOs can prescribe medications and perform surgeries.
- Residency Training: MDs and DOs complete residencies in their chosen specialties.
- Board Certification: Both MDs and DOs can become board-certified in their respective specialties.
- Continuing Education: MDs and DOs are required to complete continuing education to maintain their licenses.
- Licensure: MDs and DOs must be licensed in the state where they practice.
- Patient Population: MDs and DOs treat patients of all ages and backgrounds.
These aspects highlight the unique contributions of MDs and DOs to the healthcare landscape. Their complementary approaches provide patients with a diverse range of options to meet their individual health needs.
Education
This fundamental difference in education is a critical component of the distinction between MDs and DOs. Allopathic medical schools emphasize a traditional approach to medicine, focusing on the use of drugs and surgery to treat disease. Osteopathic medical schools, on the other hand, incorporate a holistic approach that considers the whole person, including the musculoskeletal system. This difference in education leads to distinct philosophies and practices in patient care.
For instance, DOs are trained in osteopathic manipulative treatment (OMT), a hands-on technique that uses the musculoskeletal system to diagnose and treat a wide range of conditions. This additional training allows DOs to address the root causes of illness and promote self-healing, complementing traditional medical approaches.
Understanding this difference in education is essential for patients seeking optimal healthcare. By recognizing the unique strengths of MDs and DOs, patients can make informed decisions about their medical care providers and treatment options. This knowledge empowers patients to take an active role in their health and well-being.
Osteopathic Manipulative Treatment (OMT)
Osteopathic Manipulative Treatment (OMT) is a defining characteristic that distinguishes DOs from MDs. This hands-on approach involves using the musculoskeletal system to diagnose and treat a wide range of conditions, complementing traditional medical approaches. OMT is based on the philosophy that the body has the ability to heal itself, and that by addressing the musculoskeletal system, DOs can promote self-healing and improve overall health.
- Diagnosis: DOs use OMT to assess the musculoskeletal system for misalignments, restrictions, and other abnormalities that may contribute to pain, discomfort, and dysfunction.
- Treatment: DOs use a variety of OMT techniques, such as stretching, massage, and joint manipulation, to address musculoskeletal issues, reduce pain, and improve mobility.
- Prevention: OMT can be used to prevent musculoskeletal problems by promoting proper alignment, reducing tension, and improving overall body mechanics.
- Complementary Therapy: OMT can be used in conjunction with other medical treatments, such as medication and surgery, to enhance their effectiveness and reduce side effects.
The inclusion of OMT in DOs' education and practice sets them apart from MDs and provides patients with a unique and holistic approach to healthcare. By addressing the musculoskeletal system, DOs can effectively treat a wide range of conditions, promote self-healing, and optimize overall health and well-being.
Holistic Approach
Within the realm of "difference between MD and DO," the holistic approach adopted by DOs stands as a defining characteristic. It sets them apart from MDs and shapes their unique approach to patient care. This holistic perspective encompasses several key facets, each contributing to the comprehensive and patient-centered care provided by DOs.
- Mind-Body Connection: DOs recognize the interconnectedness of the mind and body. They consider how psychological factors, such as stress and emotions, can influence physical health and vice versa.
- Focus on Prevention: DOs emphasize preventive medicine and lifestyle modifications to promote overall well-being. They believe that addressing the root causes of illness can help prevent future health issues.
- Patient-Centered Care: DOs prioritize building strong relationships with their patients. They listen attentively to their concerns, involve them in decision-making, and tailor treatment plans to their individual needs and preferences.
- Collaboration: DOs often collaborate with other healthcare professionals, such as physical therapists, nutritionists, and mental health counselors, to provide comprehensive care that addresses all aspects of a patient's health.
These facets of the holistic approach underscore the commitment of DOs to treating the whole person, not just their symptoms. By considering the mind-body connection, focusing on prevention, prioritizing patient-centered care, and collaborating with other healthcare professionals, DOs aim to optimize health outcomes and promote long-term well-being.
Scope of Practice
The scope of practice for MDs and DOs encompasses the ability to prescribe medications and perform surgeries, highlighting a crucial aspect of the "difference between MD and DO." This shared responsibility underscores their common ground as licensed physicians, equipped to provide comprehensive medical care to patients.
The ability to prescribe medications and perform surgeries is a direct result of the rigorous training and education that both MDs and DOs undergo. Medical school and residency programs provide them with the knowledge, skills, and experience necessary to diagnose and treat a wide range of conditions, including those that require surgical intervention or pharmacological management.
In practice, MDs and DOs collaborate to provide optimal care for their patients. They may consult with each other on complex cases, drawing upon their respective backgrounds and expertise. For instance, a DO with specialized training in osteopathic manipulative treatment (OMT) may provide complementary therapies to enhance recovery after surgery performed by an MD.
Understanding the scope of practice for MDs and DOs is essential for patients seeking informed healthcare decisions. It empowers them to choose providers who align with their specific needs and preferences. Moreover, it highlights the complementary nature of MDs and DOs within the healthcare system, working together to improve patient outcomes.
Residency Training
Residency training is a critical component of the "difference between MD and DO." It is during residency that both MDs and DOs receive specialized training in their chosen fields, such as internal medicine, surgery, pediatrics, or obstetrics and gynecology. This training is essential for developing the skills and knowledge necessary to practice medicine independently.
There are some key differences between MD and DO residency programs. MD residency programs are typically more focused on traditional medical treatments, such asDO residency programs, on the other hand, typically include more training in osteopathic manipulative treatment (OMT). OMT is a hands-on technique that uses the musculoskeletal system to diagnose and treat a variety of conditions.
Despite these differences, both MD and DO residency programs are designed to prepare physicians to provide high-quality patient care. Upon completing residency, MDs and DOs are eligible to sit for board certification exams in their chosen specialties.
Understanding the role of residency training in the "difference between MD and DO" is important for patients seeking healthcare. By choosing a physician who has completed an accredited residency program, patients can be confident that they are receiving care from a qualified and experienced provider.
Board Certification
Board certification is a critical component of the "difference between MD and DO." It signifies that a physician has met rigorous standards of education, training, and experience in their chosen field. Board certification is a voluntary process, but it is widely recognized as a mark of excellence in the medical profession.
There are several different organizations that offer board certification for MDs and DOs. The American Board of Medical Specialties (ABMS) is the largest and most well-known of these organizations. The ABMS certifies MDs and DOs in 24 different specialties, including internal medicine, surgery, pediatrics, and obstetrics and gynecology.
To become board-certified, MDs and DOs must complete an accredited residency program in their chosen specialty. They must also pass a rigorous written examination. Once they are board-certified, MDs and DOs must complete continuing medical education (CME) credits to maintain their certification.
Board certification is important for several reasons. First, it assures patients that their physician has met high standards of education and training. Second, it helps to ensure that physicians stay up-to-date on the latest medical advances. Third, board certification can enhance a physician's reputation and credibility.
Continuing Education
Continuing education is a critical component of the "difference between MD and DO." It is a requirement for both MDs and DOs to complete continuing education credits in order to maintain their licenses. This ensures that physicians stay up-to-date on the latest medical advances and best practices.
There are several reasons why continuing education is important for MDs and DOs. First, it helps to ensure that physicians are providing the best possible care to their patients. Second, it helps to maintain the trust between physicians and the public. Third, it helps to promote the profession of medicine.
There are many different ways for MDs and DOs to complete continuing education credits. They can attend conferences, workshops, and seminars. They can also read medical journals and books. Some states also require physicians to complete online continuing education courses.
The specific requirements for continuing education vary from state to state. However, all states require MDs and DOs to complete a certain number of credits each year in order to maintain their licenses. This ensures that physicians are staying up-to-date on the latest medical advances and are providing the best possible care to their patients.
Licensure
Within the context of "difference between md and do," licensure stands as a critical aspect that shapes the practice of medicine. It ensures that physicians meet specific standards of education, training, and ethical conduct, fostering public trust and safeguarding patient safety.
- Legal Requirement: Both MDs and DOs must obtain a license from the state medical board to practice medicine within its jurisdiction. This license serves as legal authorization to provide medical care and perform medical procedures.
- Educational Standards: Licensure requires physicians to have completed accredited medical school and residency programs, demonstrating their mastery of medical knowledge and clinical skills.
- Examination Process: To obtain a license, physicians must pass comprehensive examinations that assess their medical knowledge, clinical judgment, and ethical understanding.
- Continuing Education: License renewal typically mandates continuing medical education, ensuring that physicians stay abreast of advancements in medical science and best practices.
The licensure requirement underscores the importance of ensuring that patients receive medical care from qualified and competent practitioners. It promotes accountability, fosters public confidence, and ultimately contributes to the delivery of safe and effective healthcare.
Patient Population
Within the context of "difference between md and do," the patient population served by MDs and DOs is a significant aspect to consider. Both MDs and DOs are licensed to practice medicine and treat patients of all ages and backgrounds, including:
- Infants, children, and adolescents
- Adults
- Elderly patients
- Patients from diverse cultural and socioeconomic backgrounds
This shared patient population highlights the comprehensive nature of their medical practice. MDs and DOs are trained to diagnose and treat a wide range of medical conditions, from common illnesses to complex diseases, ensuring accessible and equitable healthcare for all.
Furthermore, the holistic approach adopted by DOs, with its emphasis on the musculoskeletal system and preventive care, complements the traditional medical approach of MDs. This collaborative approach can provide patients with a more comprehensive and individualized treatment plan, addressing both the physical and functional aspects of their health.
In exploring the "difference between md and do," we've illuminated the unique contributions of each profession to the healthcare landscape. MDs, with their emphasis on traditional medical approaches, and DOs, with their holistic approach that incorporates osteopathic manipulative treatment (OMT), offer complementary perspectives in patient care. Both are licensed physicians, completing rigorous medical training and adhering to ethical guidelines, ensuring the delivery of safe and effective medical care.
As we navigate the ever-evolving healthcare landscape, understanding the nuances between MDs and DOs empowers patients to make informed decisions about their medical care providers. The holistic approach adopted by DOs, with its focus on preventive care and the musculoskeletal system, provides a valuable adjunct to traditional medical approaches. This collaborative approach can lead to more comprehensive and individualized treatment plans, addressing both the physical and functional aspects of a patient's health.
Jeff Kay: A Versatile Actor With A Passion For Social Justice
Unveiling The Artistry Of Karina Veiga: Emotional Expressions In Abstract Art
Perrie Edwards' Height: Unveiling The Mystery


ncG1vNJzZmifoqTCsbPKZ5imq2NjsaqzyK2YpaeTmq6vv8%2Bamp6rXpi8rnvDop2fnaKau6SxjJucra%2BVmrtuucNmmKecXZm8b7TTpqM%3D